- What is Medical Software?
- Types of Medical Softwares
- Benefits of Medical Software Development for US Medical Businesses
- Top Technologies in Medical Software Development 2024
- The Process of Medical Software Development in the US
- Must-Have Features of Medical Software Development in the US
- Cost of Developing a Medical Software
- Case Study of a Popular Medical Software in US: AliveCor
- Looking to Develop Medical Software for Your Business?
- FAQs

The healthcare landscape is constantly evolving, and medical software plays a pivotal role in this transformation. From streamlining workflows for doctors to empowering patients with self-management tools, these applications hold immense potential. But have you ever wondered, “How much does it cost to develop such groundbreaking software?”
This blog post unveils the mysteries behind medical software development costs. We’ll dissect the key factors that influence the price tag and provide a roadmap for navigating the development process. Whether you’re a seasoned healthcare provider with a vision or a budding entrepreneur venturing into this exciting field, this guide will equip you with the knowledge to make informed decisions.
So, buckle up and get ready to explore the intricate world of medical software development costs!
- What is Medical Software?
- Types of Medical Softwares
- Benefits of Medical Software Development for US Medical Businesses
- Top Technologies in Medical Software Development 2024
- The Process of Medical Software Development in the US
- Must-Have Features of Medical Software Development in the US
- Cost of Developing a Medical Software
- Case Study of a Popular Medical Software in US: AliveCor
- Looking to Develop Medical Software for Your Business?
- FAQs
What is Medical Software?
Medical software has become the invisible backbone of modern healthcare, silently orchestrating a symphony of tasks behind the scenes. Its reach extends far beyond sterile clinic walls, weaving itself into the fabric of medical devices, diagnostic tools, and even wearable technology.
Source: AcumenrResearchandConsulting
At its core, medical software serves a dual purpose: enhancing patient care and streamlining healthcare operations. Here’s a glimpse into this transformative technology:
- Powering Devices and Diagnostics: Medical software isn’t just a program; it’s the brain behind many medical devices. From the intricate algorithms guiding an MRI scanner to the software embedded in a pacemaker, this technology plays a crucial role in diagnosis and treatment.
- Data-Driven Decision Making: The healthcare industry thrives on information. Medical software acts as a tireless collector, meticulously gathering patient data. This information empowers healthcare providers to make informed decisions, personalize treatment plans, and even identify potential health risks.
- Beyond the Clinic Walls: The realm of medical software extends beyond traditional healthcare settings. Wearable devices, embedded with sophisticated software programs, allow for continuous health monitoring and data collection, empowering patients to take a more active role in their well-being.
- A Diverse Ecosystem: Medical software isn’t monolithic. It encompasses a vast array of specialized programs, each catering to a specific need. Electronic health records (EHR) ensure patient information is readily available, while telemedicine platforms bridge geographical gaps, allowing for virtual consultations..
Types of Medical Softwares
The US healthcare landscape is undergoing a digital revolution, with medical software playing a central role in transforming how care is delivered and managed. Here’s a closer look at some of the most common types of medical software used in the US, along with real-world examples to illustrate their impact:
1. EHR (Electronic Health Record)/ EMR (Electronic Medical Record):
EHRs serve as a centralized digital repository for a patient’s medical history, including diagnoses, medications, allergies, immunizations, lab results, and imaging reports. EMRs typically focus on a patient’s experience within a specific practice, while EHRs aim for a more comprehensive record across different providers.
- Impact: EHR adoption in the US has grown significantly, with a 2020 ONC report indicating over 90% of hospitals using certified EHR technology. This widespread adoption has led to several benefits:
- Improved care coordination: EHRs enable seamless information sharing between healthcare providers, reducing the risk of errors and omissions due to incomplete medical histories.
- Enhanced patient engagement: Some EHR systems offer patient portals, allowing patients to view their medical records, refill prescriptions, and communicate with their doctors online.
- Streamlined workflows: EHRs automate administrative tasks like appointment scheduling and medication prescribing, freeing up valuable time for clinicians to focus on patient care.
- Case Study: The Mayo Clinic, a renowned US healthcare provider, implemented a comprehensive EHR system in 1997. This system has enabled them to improve medication safety, reduce duplicate testing, and enhance patient engagement through a secure online portal.
2. Healthcare CRM Software:
Similar to traditional CRM software used in other industries, healthcare CRM helps manage patient relationships. It tracks patient interactions, appointment history, and treatment plans, allowing providers to personalize care and improve communication.
- Impact: Healthcare CRMs are becoming increasingly popular in the US, with benefits including:
- Strengthened patient engagement: CRMs allow for targeted outreach campaigns to promote preventive care and wellness programs.
- Increased patient satisfaction: By streamlining communication and appointment scheduling, CRMs can improve the overall patient experience.
- Improved revenue cycle management: CRMs can help identify potential billing issues and streamline the claims submission process.
- Case Study: Atrium Health, a large healthcare system in the Southeast US, adopted a healthcare CRM to manage patient relationships across its network of hospitals and clinics. This system has resulted in a significant improvement in appointment scheduling efficiency and patient satisfaction.
3. Medical Billing Software:
Medical billing software automates the entire medical billing process, from generating claims to tracking payments and managing denials.
- Impact: Efficient medical billing is crucial for the financial health of US healthcare providers. Medical billing software offers several advantages:
- Reduced errors and improved accuracy: Automating claim submission reduces the risk of human error, leading to fewer denials and faster reimbursements.
- Increased revenue collection: The software can identify and address billing issues promptly, ensuring timely payments.
- Improved cash flow: Faster claims processing translates to quicker cash flow for healthcare providers.
4. Hospital Management System (HMS):
HMS is a comprehensive software suite designed to manage various aspects of hospital operations, including patient admissions, scheduling, billing, inventory management, and resource allocation.
- Impact: HMS plays a critical role in optimizing hospital workflows and improving patient care in the US. Here are some key benefits:
- Enhanced operational efficiency: HMS streamlines administrative tasks and resource allocation, leading to improved hospital efficiency.
- Reduced costs: By optimizing resource utilization and streamlining workflows, HMS can help hospitals reduce operating costs.
- Improved patient outcomes: HMS can contribute to better patient outcomes by facilitating communication between healthcare providers and ensuring timely access to necessary resources.
- Case Study: New York-Presbyterian Hospital, a leading US healthcare provider, uses a comprehensive HMS to manage its complex operations. This system has enabled them to improve patient wait times, optimize bed occupancy rates, and enhance overall operational efficiency.
5. E-Prescribing Software:
E-prescribing software allows healthcare providers to electronically transmit prescriptions directly to pharmacies, eliminating the need for paper prescriptions.
- Impact: E-prescribing is gaining traction in the US due to its numerous benefits:
- Improved medication safety: E-prescribing reduces the risk of errors associated with handwritten prescriptions, such as illegible handwriting or dosage mistakes.
- Enhanced patient convenience: Patients can receive their medications faster and more conveniently without waiting for pharmacies to decipher handwritten prescriptions.
- Streamlined workflows: E-prescribing eliminates the need for manual paperwork and streamlines the prescription process for both providers and pharmacies.
- Case Study: The Department of Veterans Affairs (VA) in the US has been a leader in e-prescribing adoption. The VA system has seen a significant reduction in medication errors and improved patient safety since implementing e-prescribing nationwide.
6. Telemedicine Software:
Telemedicine software facilitates remote healthcare consultations through video conferencing or other secure communication channels.
- Impact: Telemedicine is rapidly transforming healthcare delivery in the US, offering several advantages:
- Increased access to care: Telemedicine allows patients in remote areas or with limited mobility to access specialist care without traveling long distances.
- Improved chronic disease management: Telemedicine can be used for regular check-ins with patients managing chronic conditions, promoting better adherence to treatment plans.
- Reduced healthcare costs: Telemedicine consultations can be more cost-effective than traditional in-person visits, benefiting both patients and healthcare providers.
- Case Study: During the COVID-19 pandemic, telemedicine adoption skyrocketed in the US. Hospitals and clinics leveraged telemedicine platforms to conduct virtual consultations, reducing the risk of virus transmission and ensuring continuity of care for patients.
7. Appointment Booking Software:
Appointment booking software allows patients to schedule appointments online, reducing the need for phone calls and simplifying the scheduling process.
- Impact: Appointment booking software is becoming increasingly popular in the US healthcare system, offering benefits for both patients and providers:
- Improved patient convenience: Patients can schedule appointments 24/7 at their convenience, increasing patient satisfaction.
- Reduced administrative burden: Online scheduling frees up staff time from handling phone calls for appointments, allowing them to focus on other tasks.
- Increased appointment adherence: Online appointment reminders can help reduce the number of missed appointments.
- Case Study: Many large healthcare systems in the US, like Kaiser Permanente, have implemented online appointment booking systems. These systems have led to a significant increase in patient self-scheduling and a reduction in missed appointments, improving overall operational efficiency.
8. Medical Device Software:
Medical device software plays a critical role in the operation of various medical devices, including diagnostic equipment, monitoring systems, and even prosthetics.
- Impact: Software embedded in medical devices is essential for accurate diagnoses, effective treatment delivery, and patient monitoring in the US. Here are some key areas where medical device software is making a difference:
- Advanced diagnostics: Imaging software aids in early and accurate detection of diseases, leading to improved patient outcomes.
- Therapeutic applications: Medical device software plays a crucial role in robotic surgery, insulin pumps, and other therapeutic devices.
- Patient monitoring: Software embedded in monitoring systems allows for continuous tracking of vital signs and other patient health data, enabling timely intervention when necessary.
- Case Study: Modern medical imaging equipment like MRI scanners relies heavily on sophisticated software to generate detailed images and provide accurate diagnoses. These advancements have revolutionized medical diagnostics in the US.
9. Medical Practice Management Software:
Medical practice management software integrates various functionalities needed for smooth operation of a medical practice, including appointment scheduling, billing, electronic health records, and patient communication tools.
- Impact: Medical practice management software is a vital tool for US healthcare providers, offering numerous advantages:
- Enhanced practice efficiency: The software streamlines administrative tasks and workflows, freeing up time for clinicians to focus on patient care.
- Improved financial management: Billing and coding functionalities ensure accurate and efficient billing processes.
- Better patient communication: Integrated communication tools allow for secure communication between patients and providers, improving patient engagement.
- Case Study: Small and medium-sized medical practices across the US widely utilize medical practice management software. These software solutions help them manage their operations efficiently, improve patient care, and remain competitive in the healthcare landscape.
Benefits of Medical Software Development for US Medical Businesses
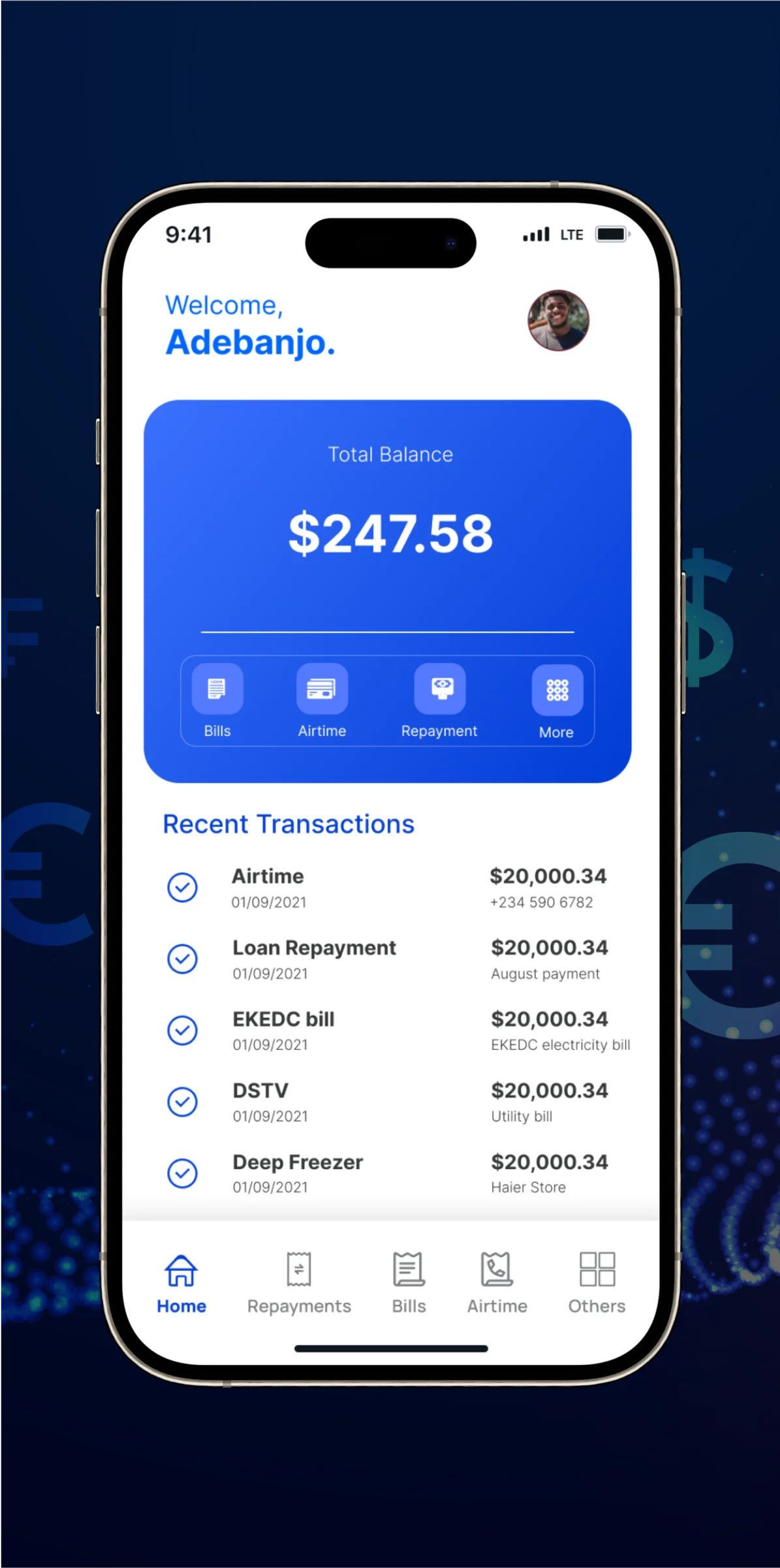
The US healthcare landscape is undergoing a digital transformation, driven by the surge of medical software development. These advancements are not just buzzwords; they translate into tangible benefits for both medical businesses and patients. Here’s a closer look at how US medical software is reshaping healthcare:
1. Enhanced Security and Privacy
Gone are the days of vulnerable paper records. Modern medical software prioritizes robust security features like multi-factor authentication and encryption. This ensures compliance with HIPAA regulations and safeguards sensitive patient information. Consider this: Baptist Health South Florida, a leading healthcare provider, recently upgraded their EHR system with enhanced security features. This system encrypts patient data at rest and in transit, exemplifying the commitment to data protection in the digital age.
2. Streamlined Workflows
Administrative tasks can devour a physician’s workday. Medical software automates these burdens, freeing up valuable time for patient care. Electronic health records (EHRs) eliminate paper charts, while automated appointment scheduling reduces administrative headaches. A study by the American Medical Association found that practices using EHRs experienced a 20% reduction in administrative tasks. Atrium Health, a large healthcare system, implemented a medical practice management software solution in 2021. This resulted in a significant improvement in workflow efficiency, allowing their medical professionals to dedicate more time to patients.
3. Advanced Diagnostics for Better Outcomes
Traditional diagnostic methods may have limitations. Medical software is changing the game with advanced diagnostic imaging systems and AI-powered analytics. EHRs offer a comprehensive view of a patient’s medical history, allowing for more informed treatment planning. For instance, Mount Sinai Hospital in New York City utilizes an AI-powered radiology platform that assists radiologists in identifying potential abnormalities in scans. This translates to earlier and more accurate diagnoses, improving patient outcomes. A 2022 Mount Sinai study using this platform successfully detected early signs of lung cancer, potentially saving lives.
4. Empowering Patients
Communication and education are cornerstones of good care. Patient portals integrated with medical software empower patients to take a more active role in their health. These portals allow secure access to medical records, test results, and online communication with doctors. Additionally, educational resources and appointment reminders delivered through medical software applications can improve patient engagement and adherence to treatment plans. The Cleveland Clinic implemented a patient portal system in 2020. Since then, they’ve reported a significant increase in patient engagement and satisfaction, highlighting the power of digital tools in fostering patient-provider collaboration.
5. Telehealth Expanding Access to Care
Limited access to healthcare, particularly in rural areas, can be a barrier to timely treatment. Telehealth platforms facilitated by medical software bridge this gap by enabling remote consultations between patients and providers. The COVID-19 pandemic propelled telehealth adoption forward. A 2021 McKinsey & Company study reported a 76% increase in telehealth utilization in the US compared to pre-pandemic levels. The Mayo Clinic, a renowned US medical institution, embraces telehealth by offering virtual consultations in various specialties, reducing travel burdens and wait times for patients.
6. Bolstered Revenue and Reduced Costs
Inefficient billing processes and manual data entry can lead to lost revenue for medical businesses. A 2023 report by the American Hospital Association estimates that US healthcare providers lose over $262 billion annually due to billing errors and inefficiencies. Medical billing software automates claim submissions and streamlines the revenue cycle, reducing errors and ensuring faster reimbursements. Additionally, by optimizing workflows through automation and reducing administrative tasks, medical software can contribute to significant cost savings.
A study by HIMSS Analytics revealed that hospitals using comprehensive EHR systems experience an average return on investment (ROI) of 300%. Parkview Health, a healthcare system, implemented a medical software solution that automated tasks and streamlined operations. This resulted in a substantial increase in revenue collection and a significant reduction in administrative costs.
7. Collaborative Care
Fragmented data systems can hinder communication and collaboration between healthcare providers, potentially leading to duplicative tests or medication errors. Medical software facilitates secure data exchange between different healthcare organizations. This allows physicians to access a patient’s complete medical history, regardless of where the care was provided.
Improved data sharing fosters better care coordination and collaboration among healthcare professionals, ultimately leading to improved patient outcomes. For instance, a multi-state healthcare system implemented a healthcare information exchange (HIE) platform that allows hospitals and clinics to securely share patient data. This has resulted in improved care coordination, reduced duplicate tests, and better overall patient management.
8. Future-Proofing Practices
The healthcare landscape is constantly evolving, with new regulations and patient needs emerging. Medical software designed with scalability and adaptability in mind allows medical practices to keep pace with these changes. Cloud-based solutions offer flexible storage and computing power, allowing medical businesses to grow without software limitations.
Additionally, regular updates ensure compliance with evolving regulations and security standards. A small pediatric practice adopted a cloud-based EHR system that is easily scalable. This allows them to add new features and functionalities as their practice grows, ensuring they can continue to meet the needs of their patients.
9. The Power of Prevention
Medical software plays a crucial role in preventive care. Advanced analytics tools can identify patients at high risk for developing certain diseases. This allows healthcare providers to implement preventive measures, such as early screenings or lifestyle modifications. For example, a healthcare system utilizes a software program that analyzes patient data to identify individuals at high risk of heart disease. Patients flagged by the system are then enrolled in preventive care programs, potentially reducing the future burden of chronic diseases.
Top Technologies in Medical Software Development 2024
The US healthcare landscape is undergoing a significant digital transformation, driven by innovative medical software development. Here’s a look at some of the top technologies shaping the future of US medical software in 2024, along with recent
1. Blockchain for Secure Data Management
Data security breaches are a major concern. Blockchain technology offers a secure and decentralized platform for storing electronic health records (EHRs). This distributed ledger system ensures data immutability and eliminates single points of failure, making it highly resistant to cyberattacks. In June 2023, a consortium of leading US healthcare providers launched a pilot program for a blockchain-based platform called “MedChain.” This initiative allows patients to control their medical data and seamlessly grant access to authorized healthcare professionals, potentially revolutionizing data security practices in the US healthcare system.
2. AR/VR for Enhanced Education and Training
Traditional patient education materials can be impersonal. Augmented reality (AR) and virtual reality (VR) provide immersive and interactive experiences. AR apps can overlay digital information onto a patient’s body, allowing them to visualize anatomy and procedures. VR simulations create realistic training environments for doctors and nurses. In August 2023, Harvard Medical School launched a new VR training program for surgical residents. These VR simulations provide a realistic and immersive learning experience, potentially improving surgical outcomes and patient safety. A JAMA study found VR training significantly improved residents’ surgical skills assessments compared to traditional methods.
4. AI Powering Diagnostics, Drug Discovery, and Personalized Medicine
Traditional diagnostic methods can be time-consuming and prone to errors. AI-powered medical software can analyze vast amounts of medical data to identify patterns and trends that might be missed by humans. This can lead to earlier and more accurate diagnoses, along with the development of more targeted and effective treatments. AI can also analyze patient data and genetic information to develop personalized treatment plans. In July 2023, the FDA approved the first AI-powered diagnostic tool for breast cancer detection. This tool, developed by a Silicon Valley startup, can analyze mammogram images with high accuracy for potential signs of cancer, potentially improving early detection rates.
5. Machine Learning (ML) for Optimized Operations and Patient Outcomes
Healthcare organizations constantly strive to improve efficiency and patient outcomes. Machine learning algorithms can analyze vast amounts of healthcare data to identify trends and patterns. This information can be used to optimize workflows, predict patient readmission risks, and identify patients who may benefit from preventive care interventions. A recent American Hospital Association study found that hospitals using machine learning to predict readmission risks reduced rates by an average of 15%. This translates to significant cost savings and improved patient outcomes. In October 2023, Cleveland Clinic partnered with a healthcare AI company to implement machine learning algorithms for predicting patient readmission risks. This initiative is expected to improve patient care coordination and reduce healthcare costs.
6. Enhanced Chatbots for Patient Communication and Care Management
Limited access to healthcare providers and long wait times can be frustrating for patients. AI-powered chatbots integrated with medical software can provide patients with 24/7 access to basic medical information, appointment scheduling, and medication reminders. These chatbots can also answer frequently asked questions and offer basic support, reducing the burden on healthcare professionals. Additionally, chatbots can be integrated with remote monitoring systems to collect patient data and provide feedback to healthcare providers, allowing for more proactive care management. The US Department of Veterans Affairs (VA) has implemented a chatbot service called “VA Bot” that allows veterans to schedule appointments, refill prescriptions, and access mental health resources. This service has improved access to care for veterans and reduced wait times.
7. Internet of Things (IoT) for Remote Patient Monitoring
Traditional methods of monitoring chronic conditions often rely on infrequent office visits, which may not capture the full picture of a patient’s health. The Internet of Things (IoT) allows for the integration of wearable devices and sensors with medical software. These devices can collect real-time patient data, such as blood pressure, heart rate, and blood sugar levels. This data can then be transmitted securely to healthcare providers, allowing them to monitor patients remotely and intervene promptly if necessary.
A growing number of US health insurance companies are offering incentives to members who use wearable devices to track their health data. This trend encourages patients to take a more active role in managing their health and provides valuable data to healthcare providers.
8. Natural Language Processing (NLP) for Streamlined Data Analysis and Improved Communication
Medical records are often filled with complex terminology and unstructured data, making it difficult for healthcare providers to extract meaningful insights. Additionally, communication gaps between patients and healthcare professionals can lead to misunderstandings and medication errors. Natural Language Processing (NLP) is a subfield of AI that allows computers to understand and interpret human language. NLP can be used to analyze medical records and extract key information, such as diagnoses, medications, and allergies. This information can then be used to populate EHRs and improve the quality of care.
Additionally, NLP can be used to develop chatbots that can communicate with patients in a more natural and engaging way. A number of US healthcare startups are developing NLP-powered tools to analyze medical records and identify potential medication errors. These tools can help to improve patient safety and reduce healthcare costs. In August 2023, researchers at Stanford University developed an NLP algorithm that can analyze doctor’s notes and identify patients at high risk of developing sepsis. This tool has the potential to improve early detection rates for this life-threatening condition.
9. Digital Therapeutics (DTx) for Personalized Treatment and Behavior Change
Traditional treatment approaches may not be effective for all patients, and adherence to medication regimens can be a challenge. Digital therapeutics (DTx) are evidence-based interventions delivered through digital platforms, such as mobile apps and websites. These interventions can be used to treat a variety of conditions, including anxiety, depression, and chronic pain. DTx programs can provide patients with personalized treatment plans, educational resources, and support tools to help them manage their health and improve their well-being.
The FDA approval process for DTx is becoming more streamlined, paving the way for the development and adoption of new and innovative digital treatment options. In July 2023, the FDA approved a DTx program for the treatment of opioid use disorder. This program combines medication-assisted treatment with a mobile app that provides patients with support tools and resources to help them stay on track with their recovery.
The Process of Medical Software Development in the US
The US medical software development landscape is a complex and highly regulated environment. Here’s a breakdown of the key steps involved in creating medical software that adheres to US regulations and meets the specific needs of the healthcare industry:
1. Define Your Target Audience and US Regulatory Landscape:
- Target Audience: In the US, medical software can cater to various audiences including hospitals, clinics, physician practices, insurance companies, and even patients themselves. Understanding their specific needs and workflows is crucial. Research common challenges faced by your target audience and how your software can address them.
- US Regulatory Considerations: The US Food and Drug Administration (FDA) regulates medical devices, including software. Depending on the software’s function and risk level, it may require FDA premarket clearance or approval. Familiarize yourself with the relevant FDA regulations (21 CFR Part 820) early on to ensure your software development process adheres to compliance standards.
2. Gather Requirements and Validate Your Product Idea:
- Market Research: Conduct thorough market research to validate your product idea. This includes analyzing existing medical software solutions, identifying unmet needs, and understanding the competitive landscape.
- Needs Assessment: Engage with potential users in the US healthcare system, such as doctors, nurses, or healthcare administrators. Conduct focus groups or user interviews to gather detailed requirements and ensure your software addresses their pain points.
3. Design a User-Centered Prototype:
- User Interface (UI) and User Experience (UX) Design: Prioritize user-friendliness and compliance with US regulations like HIPAA (Health Insurance Portability and Accountability Act) for data privacy. The UI should be intuitive and minimize the risk of errors in a fast-paced healthcare environment.
- Prototyping Tools: Utilize prototyping tools to create a working model of your software. This allows for early user testing and feedback to refine the design before significant development begins.
4. Develop Your Final Prototype and Leverage US-Specific Technologies:
- Agile Development: Consider adopting an agile development methodology for iterative development and testing cycles. This allows for continuous improvement based on user feedback and ensures the final product aligns with US healthcare needs.
- HIPAA Compliance: Integrate features that ensure compliance with HIPAA regulations throughout the development process. This includes robust data security measures, access controls, and patient data encryption.
5. Coding and Development:
- Software Development Kits (SDKs): Utilize pre-built US-compliant SDKs or libraries to streamline development and ensure adherence to relevant standards.
- Development Teams: Assemble a development team with expertise in medical software development best practices and familiarity with US regulatory requirements.
6. User Testing and Refinement:
- User Acceptance Testing (UAT): Conduct thorough UAT with real users in a simulated US healthcare environment. This helps identify usability issues, ensure the software meets user needs, and verifies regulatory compliance.
- Iterative Refinement: Based on user feedback, refine the software and address any identified bugs or usability issues.
7. Deployment and Delivery:
- Deployment Strategy: Develop a deployment strategy that adheres to US healthcare IT infrastructure considerations. This may involve cloud-based deployment or on-premise solutions depending on the specific needs.
- Documentation and Training: Provide comprehensive user guides, training materials, and ongoing support to ensure US healthcare professionals can effectively utilize the software.
8. Maintenance and Post-Market Surveillance:
- Software Updates: Implement a plan for ongoing software updates, bug fixes, and security patches to maintain functionality and address any emerging threats.
- Post-Market Surveillance: Continuously monitor the software’s performance and user feedback in the US market. This helps identify any adverse events or unintended consequences and allows for proactive adjustments to ensure patient safety and regulatory compliance.
Must-Have Features of Medical Software Development in the US
Medical software plays a vital role in the US healthcare system, streamlining workflows, improving patient care, and ensuring regulatory compliance. Here’s a breakdown of essential features for successful medical software development in the US:
1. Robust Patient Tracking and Data Management:
- Vital Signs Monitoring: Track and record essential vitals like heart rate, blood pressure, blood sugar, and weight. Integrate wearable devices for real-time data capture, allowing for proactive health management.
- Electronic Health Records (EHR): Implement a comprehensive EHR system that securely stores patient medical histories, allergies, medications, and immunization records. Ensure compliance with HIPAA regulations for data privacy and security.
- Clinical Decision Support (CDS): Incorporate CDS tools to provide evidence-based recommendations during patient care. This can help improve diagnosis accuracy and treatment recommendations.
A 2023 study published in the Journal of the American Medical Association (JAMA) found a significant improvement in patient outcomes in US hospitals that adopted EHR systems. The study linked EHR use with a decrease in hospital-acquired infections and medication errors.
2. Streamlined Appointment Scheduling and Reminders:
- Online Appointment Booking: Allow patients to schedule appointments, reschedule, or cancel bookings conveniently through an online portal or mobile app.
- Automated Reminders: Implement automated appointment reminders via email, text message, or phone calls to reduce patient no-shows and improve appointment efficiency.
3. Efficient Insurance Processing and Billing:
- Integrated Billing System: Integrate an automated billing system that handles insurance claims processing, eligibility verification, and co-pay calculations. This can expedite claim reimbursements and reduce administrative burdens for healthcare providers.
- Real-time Eligibility Verification: Enable real-time insurance verification to ensure accurate billing and minimize claim denials.
4. Secure E-Prescribing:
- E-Prescribing Integration: Integrate e-prescribing functionalities to allow physicians to send prescriptions electronically to pharmacies, improving medication accuracy and reducing the risk of errors associated with handwritten prescriptions.
A 2022 study by the Centers for Disease Control and Prevention (CDC) found that e-prescribing significantly reduced medication errors in the US healthcare system. The study linked e-prescribing with a 48% decrease in overall medication errors and a 67% decrease in dispensing errors.
5. Interoperable Data Sharing:
- HL7 FHIR Integration: Implement interoperability standards like HL7 FHIR to facilitate secure data exchange between different healthcare software systems. This allows for seamless information sharing between hospitals, clinics, and pharmacies, improving care coordination and patient outcomes.
6. Mobile Accessibility:
- Mobile-Friendly Design: Develop a mobile-friendly version of your software or a dedicated mobile app for physicians and other healthcare providers to access patient records, schedule appointments, and manage tasks on the go.
7. Secure Cloud-Based Solutions:
- Cloud-Based Deployment: Consider cloud-based deployment options for scalability, data accessibility, and disaster recovery. Ensure the cloud provider adheres to HIPAA compliance regulations for data security.
8. Integration with Telehealth Tools:
- Telehealth Integration: Integrate telehealth functionalities to enable virtual consultations between patients and healthcare providers. This can improve access to care, especially in underserved areas.
9. Advanced Analytics and Reporting:
- Data Analytics Integration: Integrate data analytics tools to generate reports on patient demographics, treatment trends, and resource utilization. This data can be used to improve healthcare delivery, identify cost-saving opportunities, and make data-driven decisions.
Cost of Developing a Medical Software
| Step | Description | Estimated Cost Range (USD) |
| 1. Research & Planning | Market research, defining target audience, regulatory research | $5,000 – $20,000 |
| 2. Design & UI/UX | Prototyping, user experience research, workflow development | $10,000 – $30,000 |
| 3. Front-End Development | Programming UI for web/mobile app, implementing functionalities | $15,000 – $50,000 |
| 4. Back-End Development | Server-side development, integration with databases and systems | $20,000 – $100,000+ |
| 5. Features and Integrations | Implementation of various features and integrations (e.g., scheduling, telehealth) | $10,000 – $200,000+ |
| 6. Testing and QA | Functionality, usability, security testing | $10,000 – $30,000 |
| 7. Deployment and Maintenance | App store deployment fees, server hosting, ongoing maintenance | $5,000 – $20,000+ |
| Total Estimated Cost: | ||
| Simple App | Basic app with essential features | $65,000 – $150,000 |
| Medium Complexity App | Moderate complexity, additional features | $100,000 – $300,000+ |
| Complex App (EHR system) | Comprehensive EHR system with advanced functionalities and integrations | $500,000 – $1,000,000+ |
Variable Cost Factors
Beyond the core development phases, a multitude of variable cost factors lie in wait, presenting both opportunities for optimization and potential pitfalls for the unwary. Here, we delve deeper into these key considerations to shed light on the true cost landscape:
1. The Feature Facet: Complexity Breeds Cost
The very features that imbue your software with value – appointment scheduling, patient record management – can significantly impact the development budget. Simple functionalities require less development time and resources, translating to a lower cost. However, as you venture into the realm of advanced features like AI-powered diagnostics or telehealth integrations, complexity rises proportionately, demanding a larger investment in development expertise and time.
2. Navigating the Regulatory Maze: FDA and Compliance
The US Food and Drug Administration (FDA) acts as a guardian of patient safety, dictating the level of compliance required for medical software. Software deemed high-risk by the FDA will necessitate stricter testing procedures and more rigorous documentation, inevitably increasing development costs. A thorough understanding of FDA regulations at the outset is paramount for accurate cost forecasting.
3. The Team Terrain: Location and Experience
The geographical location of your development team plays a crucial role. While hiring developers within the US often translates to a higher price tag, it comes with the advantage of clear communication and a deeper understanding of US healthcare regulations. Outsourcing to other regions might offer cost savings, but careful consideration must be given to potential communication barriers and the team’s expertise in navigating the nuances of the US healthcare system.
4. Development Methodologies: Agile Adaptation vs. Waterfall Rigidity
The chosen development methodology can influence cost control. Agile methodologies, where features are developed and tested in iterative cycles, allow for adaptation based on user feedback. This flexibility can help mitigate the need for costly rework later in the development process. Waterfall methodologies, on the other hand, plan the entire development process upfront with limited room for changes. While seemingly cost-effective initially, significant changes later in the project can lead to higher overall costs.
5. Integration Intricacies: Connecting the Healthcare Ecosystem
Integrating your medical software with existing Electronic Health Record (EHR) systems or other healthcare IT infrastructure can be a complex and potentially expensive undertaking. The level of customization and compatibility required will significantly impact the cost. A clear understanding of the existing healthcare IT landscape and the desired level of integration is essential for accurate cost estimation.
6. Security and Encryption: The Bedrock of Trust
In the realm of medical software, robust security features and data encryption are not optional – they are fundamental to ensuring patient privacy and complying with HIPAA regulations. Implementing these features requires specialized expertise and can add to the development cost. However, the potential consequences of a security breach far outweigh the initial investment.
Case Study of a Popular Medical Software in US: AliveCor
AliveCor, a leading US digital health company headquartered in Santa Clara, California, has revolutionized cardiac arrhythmia detection with its flagship product, the KardiaMobile. This single-lead ECG device attaches to a smartphone and allows users to capture a medical-grade EKG in 30 seconds.
Impact on Patients:
- Early Detection: Traditionally, diagnosing arrhythmias like atrial fibrillation (AFib) often relied on infrequent doctor visits or cumbersome 24-hour Holter monitors. KardiaMobile empowers patients to take control of their heart health by enabling them to capture EKG readings anytime, anywhere. This can lead to earlier detection of AFib, a condition that increases stroke risk by fivefold.
- Improved Management: AliveCor’s app analyzes the EKG and provides instant feedback on heart rhythm normality. This allows patients to better understand their condition and work with their doctors to manage it effectively.
- Reduced Anxiety: For people experiencing heart palpitations or other concerning symptoms, KardiaMobile offers a quick and convenient way to check their heart rhythm, potentially reducing unnecessary anxiety and emergency room visits.
Impact on Healthcare System:
- Cost Reduction: Early detection and management of AFib can significantly reduce healthcare costs associated with strokes and other complications. Studies suggest KardiaMobile can lead to a 50% reduction in unnecessary hospitalizations for suspected AFib. A recent Cleveland Clinic study published in the Journal of the American College of Cardiology found that AliveCor’s AI was as effective as doctors in detecting AFib.
- Improved Efficiency: By enabling remote monitoring and early diagnosis, AliveCor helps streamline the diagnostic process for doctors, freeing up valuable time for consultations and treatment.
- Telehealth Integration: AliveCor integrates seamlessly with telehealth platforms, allowing doctors to remotely review patients’ EKG readings and provide timely consultations, particularly beneficial in underserved areas. This is especially significant as the US healthcare system grapples with a growing physician shortage.
Challenges and the Road Ahead:
AliveCor faces competition from tech giants like Apple with their Apple Watch ECG feature. However, AliveCor is at the forefront of regulatory approvals and clinical research, constantly innovating its technology and expanding its product line. A recent patent dispute with Apple highlights the ongoing battle for dominance in this rapidly evolving market.
Recent News:
- In a major win for global accessibility, AliveCor recently announced its entry into the Indian market with the KardiaMobile 6L, the world’s only FDA-cleared six-lead personal ECG device. This expansion aims to address the critical need for affordable and convenient cardiac care in regions with limited access to traditional healthcare facilities.
- AliveCor continues to garner recognition for its innovation. The company was recently honored with an Inc. 2023 Best in Business Award and a Fast Company’s World Changing Ideas Award 2023, solidifying its position as a leader in digital health transformation.
Looking to Develop Medical Software for Your Business?
The US healthcare system craves innovation. Idea Usher delivers. We’re a medical software development powerhouse, combining expert engineers with healthcare IT specialists and regulatory gurus. We understand the intricacies of the US landscape, from HIPAA to FDA regulations. Our focus? Developing secure, user-friendly software that empowers providers and improves patient care.
Why Idea Usher? We have a proven track record of delivering cutting-edge solutions for US healthcare institutions. We leverage AI, blockchain, and cloud computing to create future-proof software. Our agile development ensures your software perfectly aligns with your needs and evolves alongside your business goals. With transparent communication, we keep you informed and involved every step of the way.
Unlock the future of US healthcare. Let Idea Usher be your partner. Contact us today for a free consultation and see how we can transform your vision into reality, optimizing healthcare delivery and revolutionizing patient care in the US.
FAQs
Q1: What does a medical software developer do?
A1: Medical software developers create and maintain software applications specifically designed for the healthcare industry. This can involve anything from Electronic Health Record (EHR) systems used by doctors and nurses to mobile apps for patient appointment scheduling and medication management. They ensure these programs are user-friendly, secure, and compliant with healthcare regulations.
Q2: How much does it cost to develop a medical app?
A2: The cost of developing a medical app can vary greatly depending on factors like complexity, features, and regulatory compliance needs. A simple app might cost around $10,000, while a complex EHR system could reach $1 million or more.
Q3: What software do medical coders use?
A3: Medical coders use specialized software programs to translate medical diagnoses and procedures into standardized codes for insurance billing purposes. These programs often include extensive medical terminology libraries and logic rules to ensure accurate coding. Some popular examples include EncoderPro, 3M Codify, and Optum CodeWarrior.
Q4: What software do most hospitals use?
A4: Hospitals typically utilize a suite of integrated software solutions to manage various aspects of their operations. This may include Electronic Health Record (EHR) systems for patient records, Enterprise Resource Planning (ERP) for financial management, and Practice Management software for scheduling and billing. Specific vendors may vary, but some of the leading players include Epic Systems, Cerner, and McKesson.