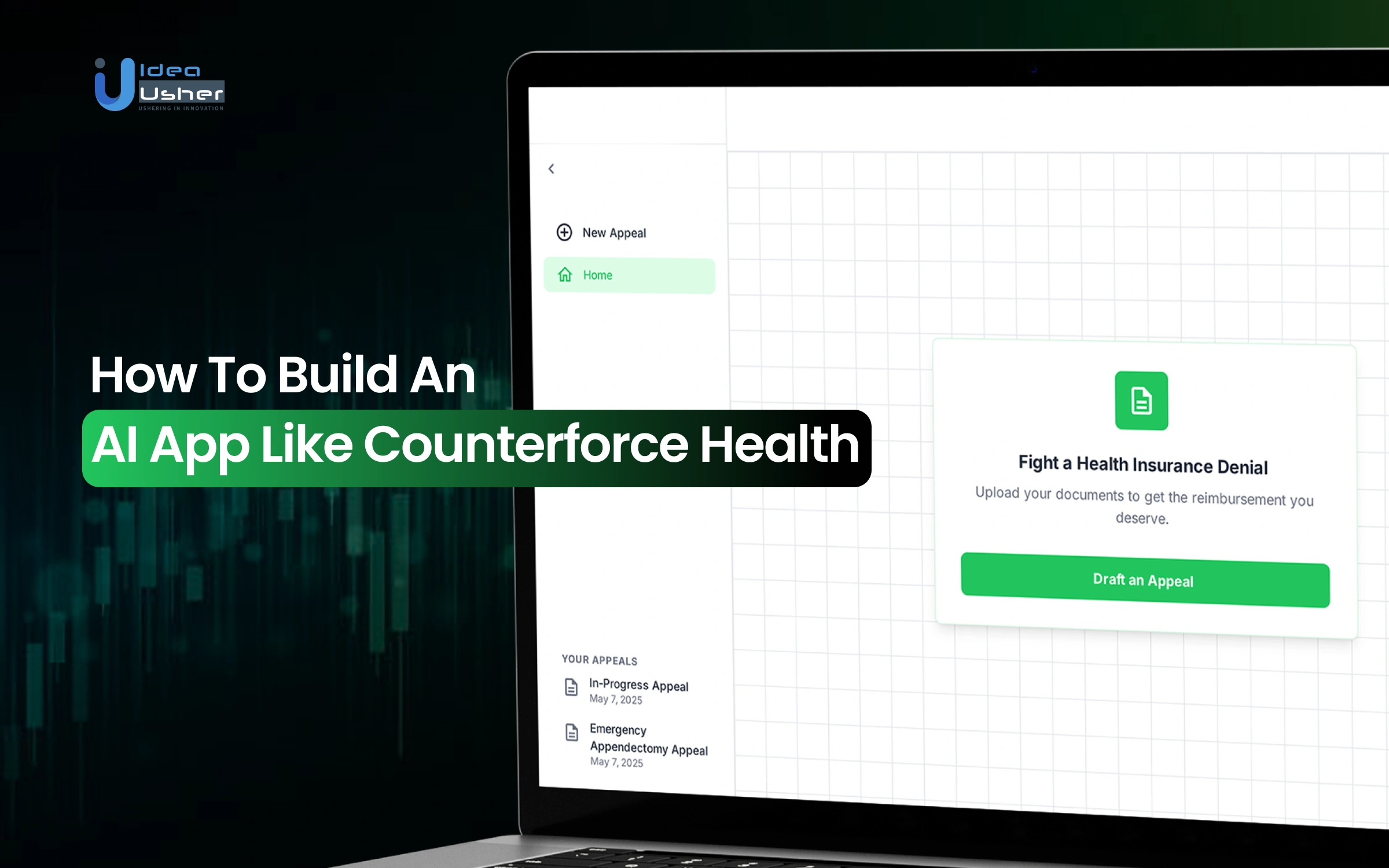
Healthcare has always been weighed down by paperwork and insurance hurdles but insurance denials can be especially frustrating. Many patients feel lost in a maze of phone calls and confusing letters. These challenges often leave them frustrated and unsure of how to navigate the system. However, AI apps like Counterforce Health are helping to change that. By allowing patients to upload their denial letters and medical records, the platform quickly generates strong, evidence-backed appeals. In just minutes, patients can access legal-grade documents that help them fight back. With expert support and community-driven initiatives, this technology makes the process simpler and more accessible.
In this blog, we’ll walk you through the process of building an AI-driven app like Counterforce Health. We’ll cover everything from key features and the tech stack to development costs and strategies for real-world implementation.
Over the past decade, we’ve developed several unique patient advocacy solutions that use NLP for analyzing and interpreting insurance claim data and ML for building intelligent appeal systems. Using this expertise, IdeaUsher can help healthcare enterprises build an AI app similar to Counterforce Health, which increases the chances of successful insurance claims for the patients.
Key Market Takeaways for AI Patient Advocacy Platform
According to GrandviewResearch, the AI in patient engagement market, valued at USD 6.08 billion in 2023, is growing quickly as healthcare shifts toward more personalized and patient-centered care. With an expected CAGR of 21.2% through 2030, AI-powered patient advocacy platforms are helping bridge the gap between patients and healthcare providers. These tools make it easier for people to understand their conditions, find credible information, and access support when they need it most.
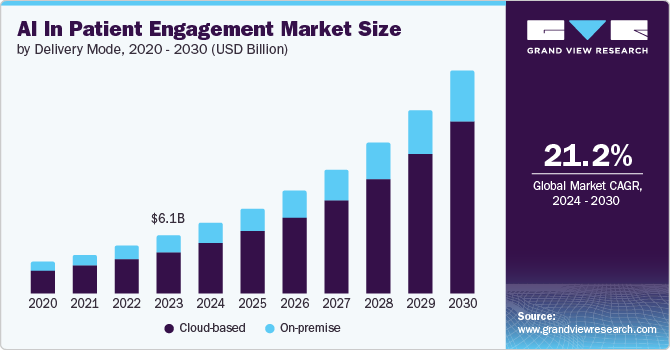
Source: GrandviewResearch
For example, platforms like Claimable automate the health insurance appeal process by guiding users through documentation, identifying likely reasons for claim denials, and helping them draft persuasive appeal letters. This automation saves patients time while improving their chances of success.
Similarly, Fight Health Insurance offers chatbot-driven support to generate personalized appeal letters from uploaded denial documents. Together, these platforms show how AI is transforming patient advocacy, making the process clearer, faster, and more equitable for people seeking fair coverage and support.
What is the Counterforce Health App?
Counterforce Health is an AI–powered advocacy platform designed to help patients and healthcare providers quickly and effectively challenge denied insurance claims. It uses advanced AI models trained on medical, legal, and claims data to analyze denial letters and insurance policies, then instantly generates a precise, evidence-backed appeal letter.
Here are some of its key features that make it stand out,
1. AI vs. AI Advocacy
Counterforce Health is built as a direct countermeasure to the automation tools insurance companies use to reject claims. Its technology identifies weak or unlawful denials and formulates a tailored response designed to meet regulatory, legal, and medical standards.
2. Instant, Personalized Appeal Letters
The core feature is its automated appeal generator. Users upload denial documents, relevant medical records, and their insurance policy. Within minutes, the system produces a professional, case-specific appeal letter, saving patients and clinics hours of manual research and writing.
3. Legal-Grade Case Building
The platform’s AI is trained on medical literature, insurance review precedents, and legal databases of successful appeals. It cites peer-reviewed medical studies and highlights policy violations, creating a fact-driven argument that’s difficult for insurers to dismiss.
4. Maxwell AI Assistant for Follow-Up
Counterforce includes Maxwell, an AI voice assistant that can contact insurance companies on a user’s behalf. Maxwell navigates phone systems, requests updates, and documents follow-up calls, reducing the time and stress patients spend dealing with bureaucratic processes.
5. High Success Rate
Counterforce Health reports overturning 70–80% of denials on first appeal, that is significantly higher than the industry average for manual appeals. This performance makes it one of the most effective claim advocacy tools currently available.
7. Technical and Timeliness Errors
The AI doesn’t just check if a treatment is medically needed. It also carefully reviews each claim for small errors or missed deadlines that could quickly turn a denial into an approval.
What is the Business Model of the Counterforce Health App?
Right now, the Counterforce Health App is completely free for patients and even for clinics that choose to use it. The team wants to grow with purpose before adding any paid plans. Over time, the model will likely shift toward steady revenue from healthcare partners while still keeping access free for individuals.
Counterforce’s revenue model is designed to scale gradually, starting with grant-backed growth and transitioning to recurring B2B revenue from healthcare organizations.
A. B2B Subscription Model (Primary Monetization)
The company’s main long-term revenue driver will come from a subscription-based platform for clinics and private practices.
- Pricing Approach: Subscription fees will be set on a per-physician or per-practice basis, often linked to the amount of revenue recovered through the platform.
- Value Proposition: Clinics gain access to automated appeal generation, analytics dashboards, and AI-driven denial pattern insights, tools that directly translate into recaptured income.
This model ensures that the end-user (patients) continue to receive free access while the financial burden shifts to the providers who derive measurable ROI.
B. Grant and Award Funding (Early-Stage Support)
To maintain free access during its growth phase, Counterforce has relied on non-dilutive grant funding and competition awards:
- $2.47 million PennAITech Grant from the University of Pennsylvania
- $5,000 Top Prize and Audience Choice Award at Grep-a-Palooza (June 2025)
- $5,000 Prize at The Launch Place’s IdeaFest (April 2025)
This funding structure allows the team to focus on product development and impact metrics before commercializing its B2B platform. The founders have also indicated an intent to continue pursuing competitive grants to expand access and support future R&D.
C. Future Revenue Streams (Strategic Growth)
Counterforce is quietly building a powerful anonymized dataset that tracks how and why insurance claims get denied across the country. Over time, it could be shared with researchers and policy groups who might use it to fix deeper issues in healthcare. This approach would also create steady ethical revenue while keeping every patient’s privacy fully protected.
Performance Metrics and Market Impact
- Success Rate: 70–80% claim reversal rate
- Time Efficiency: Reduces appeal preparation from days to under 8 minutes
- Financial Impact: Over $12 million in insurance coverage recovered for users in 2024
- Market Opportunity: A $1 trillion U.S. denial market, with over 850 million claims denied annually, and less than 1% ever appealed
This positions Counterforce as both a socially impactful tool for individuals and a financially strategic asset for providers.
Other Revenue Models for an AI Patient Advocacy App
The goal of an AI patient advocacy app should be to help people fight for fair healthcare while staying financially strong. Depending only on grants might slow growth and limit new ideas. To stay true to its mission, the platform could wisely explore different revenue models that genuinely support long-term impact.
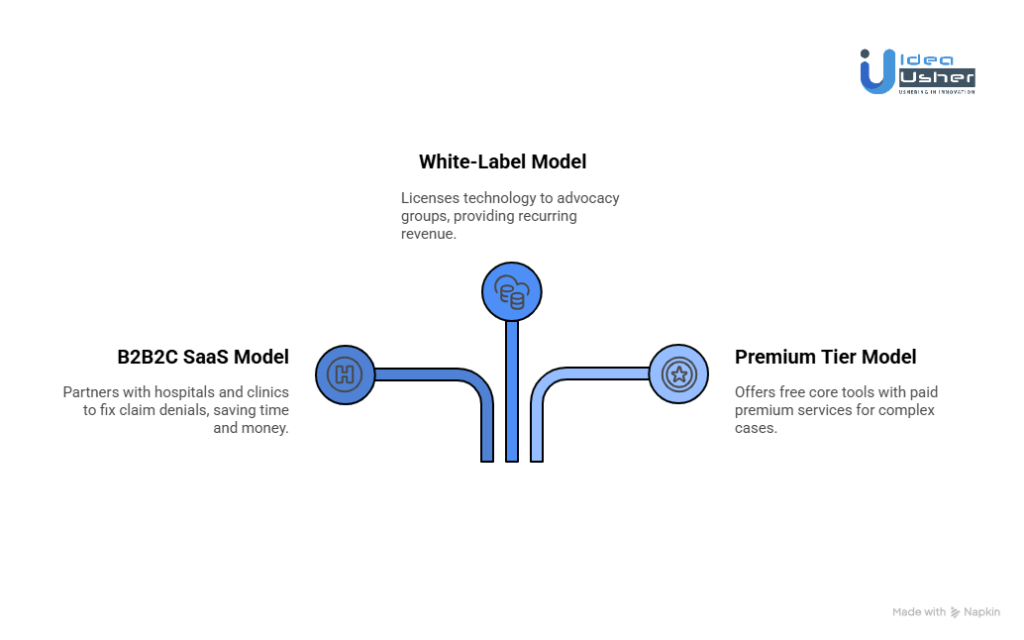
1. The B2B2C SaaS Model
Instead of billing patients, the platform could partner with hospitals and clinics that already need to fix claim denials. It might work as a Denial and Appeal Management Platform that lets staff upload denial letters in bulk and track each appeal easily. With its AI tools, they would quickly generate clear and compliant appeal drafts that save both time and money.
The Problem
- Physicians spend roughly 16 hours per week navigating payer regulations.
- The average annual cost per physician for administrative compliance exceeds $99,000.
- Each manual appeal can cost $75–$150 in staff time.
The Value Proposition
AI can cut appeal generation time by over 70%, lowering per-appeal costs to a fraction of manual methods, while improving success rates and staff satisfaction.
Pricing Structures
- Per-Appeal Fee: $25–$50 per appeal generated.
- Tiered Subscription: $499–$1,999/month based on clinic size or volume.
- “Revenue Recovery” Fee: 5–15% of recovered revenue, directly aligning incentives.
Market Validation
Companies like Cedar and PayZen show that hospitals will pay for technology that improves revenue cycle management and patient engagement. A patient advocacy platform can fit seamlessly into this existing RCM ecosystem, solving a high-cost pain point while keeping patient access free.
2. The White-Label / Co-Branded Platform Model
Many advocacy groups, medical societies, and legal organizations want to offer patient support but lack AI infrastructure. A white-label model allows them to license the technology and brand it as their own — while the platform handles the AI backend and maintenance.
Potential Partners
- Patient advocacy nonprofits
- Specialty medical societies (e.g., oncology, mental health)
- Healthcare-focused law firms
Pricing Structures
- Annual Licensing Fee: $250,000–$1 million+, depending on size and user base.
- Per-User/Per-Use Fees: For smaller partners or pilot programs.
This model provides predictable, recurring revenue and accelerates market penetration through trusted intermediaries. It’s the same approach fintech pioneers like Plaid and Health Gorilla used, powering ecosystems rather than competing within them.
3. The Premium Tier Model
Keep the core AI advocacy tools free for all users, but offer premium tiers for individuals facing high-stakes or complex denials. This cross-subsidy structure ensures accessibility while generating sustainable revenue.
Premium Services
- Expert Review: Human advocates or paralegals refine AI-generated letters.
- Full-Service Management: Platform staff handle the entire process like submissions, communications, and regulatory escalation.
- Legal Support: Optional consultation with insurance law specialists.
Pricing Options
- Expert Review: $75–$150 per appeal.
- Full-Service Management: $250–$500+ per case (with potential success guarantee).
- Membership: $19.99/month for ongoing access and support.
For a patient appealing a $50,000 denied surgery, a few hundred dollars for professional assistance is a small, rational investment in peace of mind and potential success.
Market Proof
Platforms like Rocket Lawyer and LegalZoom show the viability of the “free core, paid expert” model. The blend of AI precision with human oversight aligns perfectly with the emotional and regulatory complexity of healthcare advocacy.
How the Counterforce Health App Works?
The Counterforce Health app helps users fight insurance denials by turning their documents into strong appeal letters. It quickly analyzes details and builds clear arguments that users can review before sending. This way, they can confidently challenge unfair decisions and focus on healing.
Step 1: Users Onboard Their Case
The journey begins when a patient, caregiver, or clinic staff member visits the Counterforce Health website.
Upload the denial letter
Users upload a clear copy of their Explanation of Benefits —the insurer’s notice explaining why a claim was denied. Common reasons include phrases like “not medically necessary,” “experimental,” or “out of network.”
Add supporting documents
Users can also upload insurance plan details, medical records, or any previous correspondence. The more context provided, the stronger the appeal becomes.
This first step gives the AI system all the essential pieces it needs to begin building the case.
Step 2: The AI Advocate Gets to Work
Once the documents are submitted, Counterforce Health’s specialized AI engine begins analyzing the case.
Understanding the documents
Using advanced natural language processing, the system reads and extracts key details from denial letters and supporting materials, such as the patient’s information, relevant CPT or ICD-10 codes, the stated reason for denial, and specific policy clauses.
Strategic analysis
The AI then compares this information to its extensive database of successful appeals, medical guidelines, and insurance rules. It determines the most effective medical and legal strategy to overturn the denial.
This stage is where the AI transforms raw paperwork into actionable insight—grounded in evidence, not guesswork.
Step 3: Building a Persuasive Appeal
Next, the AI constructs a clear, evidence-based appeal letter. It uses a method called Retrieval-Augmented Generation to gather authoritative data from multiple sources:
- Medical Evidence: The system pulls from peer-reviewed journals and clinical guidelines to prove that the denied treatment is medically appropriate and standard of care for the user’s condition.
- Legal and Policy References: It identifies relevant state and federal regulations, such as the No Surprises Act, and even quotes the insurer’s own policy language to demonstrate where coverage should apply.
- Historical Precedents: It draws from patterns in thousands of prior appeals, learning which arguments and formats are most persuasive.
The result is a professionally structured, customized appeal letter ready for user review.
Step 4: Human Oversight and Final Submission
Counterforce Health is designed around collaboration between humans and AI. After the system generates the appeal:
Users stay in control. The draft letter is returned to the user (or their advocate) for review. Users can refine the tone, add personal context, or make final edits before submission.
Future automation
The company is also developing “Maxwell,” a voice-based AI assistant that will be able to call insurance companies, navigate phone menus, and check appeal statuses, saving users hours of administrative effort.
Step 5: Shifting Focus Back to Healing
Once the appeal is sent, Counterforce Health handles the complexity so users can refocus on recovery. The platform’s mission is simple:
- Reduce stress: The tedious paperwork is off users’ plates.
- Increase success: Internal data shows users’ appeals succeed at roughly twice the national average, demonstrating real-world impact.
- Empower advocacy: Every successful case strengthens the system’s ability to help the next person in need.
How to Build an AI App Like Counterforce Health?
We build AI-powered patient advocacy platforms that work in real healthcare settings. We’ve developed several apps like Counterforce Health for our clients, each designed to make advocacy faster, smarter, and more secure while keeping patient privacy at the core.
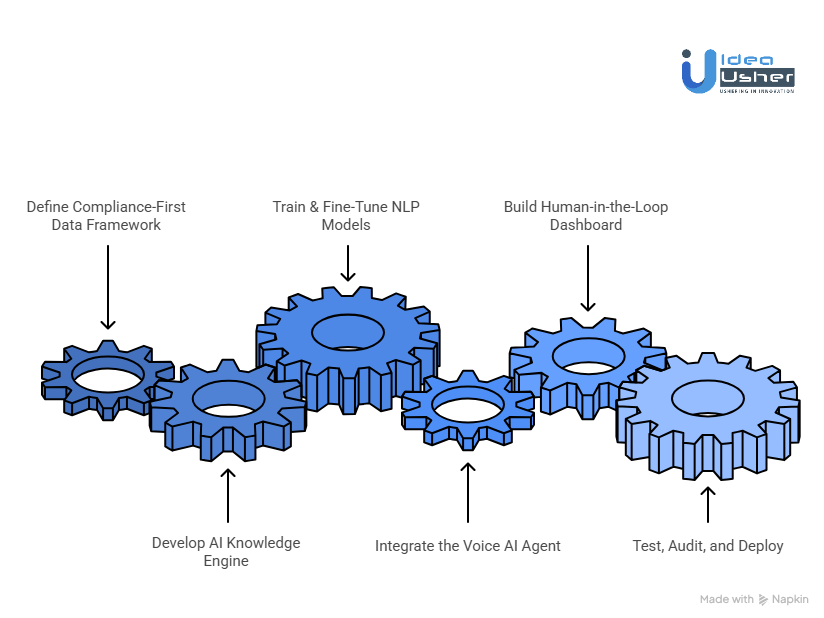
1. Define Compliance-First Data Framework
We start by mapping out where your data comes from and how it moves. This includes denial letters, EOBs, policy documents, and clinical databases. Once that’s clear, we set up a HIPAA-compliant cloud system so your data stays safe and accessible. This step builds a secure base that everything else depends on.
2. Develop AI Knowledge Engine
Next, we create a knowledge engine that can understand and connect information from different sources. We use a mix of retrieval systems and knowledge graphs so the platform can pull accurate insights quickly. With vector databases like Pinecone or Weaviate, it can find what it needs in seconds and respond in a way that feels natural.
3. Train & Fine-Tune NLP Models
We then train language models on real appeal cases and insurer documentation. Each model learns the tone and structure used in successful advocacy. We fine-tune it to understand the terms and patterns that matter most to your organization. This helps the system write letters and responses that sound professional and get results.
4. Integrate the Voice AI Agent
After that, we bring in the voice layer. Using platforms like Dialogflow or Deepgram, we build an agent that can handle calls, check claim status, and escalate issues when needed. It works like a smart assistant that can take pressure off your team and help patients get answers faster.
5. Build Human-in-the-Loop Dashboard
We believe humans should always stay in control, so we design a dashboard that keeps advocates and clinicians involved. They can review, edit, and approve every piece of AI-generated content. The dashboard also tracks quality and feedback, so the system keeps learning and improving.
6. Test, Audit, and Deploy
Finally, we test everything. We run compliance checks, security reviews, and bias audits to make sure the platform performs the way it should. Once it’s ready, we roll it out in phases, usually starting with a small pilot group. This way, we can fine-tune the platform before scaling it to more users.
Common Challenges of an AI App Like Counterforce Health
We’ve helped many clients build AI apps like Counterforce Health, and we know exactly where things can go wrong. At Idea Usher, we actually create systems that can adapt, perform reliably, and stand strong in the real world.
Challenge 1: Data Fragmentation
AI systems live or die by their data. For a health advocacy platform, the goldmine lies in detailed insurance appeals, denial letters, and payer-specific policy language. Unfortunately, this data is highly sensitive, fragmented, and locked across insurers, hospitals, and law firms.
Our Solution: Strategic, Multi-Channel Data Acquisition
We tackle data scarcity from multiple angles to help clients build strong, compliant foundations from day one:
- Partnerships with Advocacy Organizations: We collaborate with patient advocacy groups that possess anonymized historical case data aligned with your mission.
- Clinic Data Agreements: We help negotiate secure, HIPAA-compliant access to anonymized appeal data from clinics and hospitals, turning administrative pain points into valuable AI training inputs.
- Synthetic Data Generation: Using advanced generative techniques, we produce realistic, high-quality synthetic data that reflects the complexity of real appeals — without compromising patient privacy.
Challenge 2: Navigating Legal Ambiguity
An AI that drafts insurance appeal letters sits close to the boundary of “legal advice.” Without careful handling, it can expose your company to accusations of unauthorized legal practice.
Our Solution: Human-in-the-Loop Compliance by Design
We design systems that empower, not replace, human expertise:
- Transparent Draft Labeling: Every AI-generated document is clearly marked as a “Draft Appeal Letter,” helping manage user expectations and reduce legal exposure.
- HITL Review Flows: Certified patient advocates, legal specialists, or users themselves review and finalize each appeal. The AI suggests; the human decides.
Challenge 3: Building Trust and Transparency
Users won’t rely on a “black box” AI to handle appeals that could determine thousands of dollars in care coverage. Without explainability, adoption and retention both fail.
Our Solution: Explainability Baked Into the UX
We make every AI decision traceable and verifiable:
- Citation Transparency: Each claim or recommendation is backed by explicit references, from policy clauses, peer-reviewed studies, or government regulations.
- Oversight Dashboards: For enterprise clients, we build dashboards that track model performance, appeal success rates, and review outcomes, ensuring the system earns trust over time.
Challenge 4: Model Drift
Healthcare and insurance rules evolve constantly. What works today may fail tomorrow. Over time, even the best AI models lose accuracy as medical guidelines, policy wording, and laws shift.
Our Solution: Continuous Learning Infrastructure
We future-proof your AI through adaptive learning:
- Automated Retraining Pipelines: Models are periodically retrained with fresh appeal outcomes and updated policy data.
- Feedback-Driven Improvement: Every user interaction, especially successful or denied appeals, feeds directly into retraining workflows, ensuring ongoing accuracy and a strong competitive edge.
Tools & APIs for an AI App Like Counterforce Health
If you are building an AI health app, you will probably need tools that can train models, connect data, and run securely on the cloud. You might also want APIs that handle user input quickly and frameworks that make testing and updates easier.
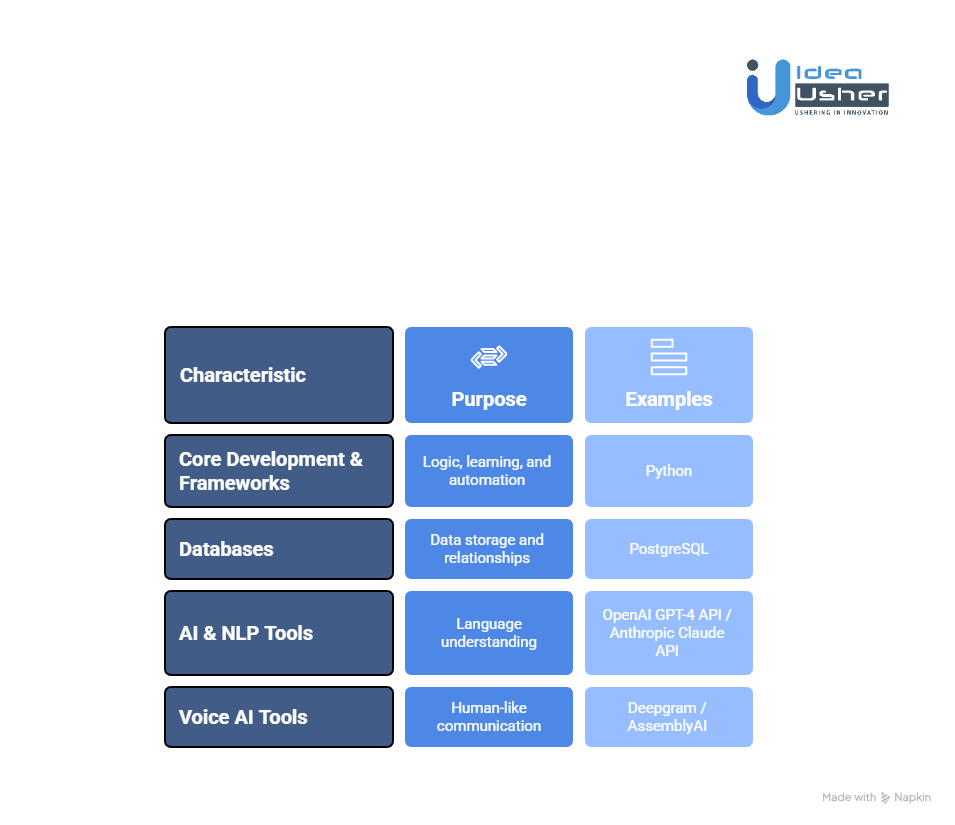
1. Core Development & Frameworks
This is the intelligence core where logic meets learning and automation works quietly in the background. It might not look flashy but it could easily become the part that makes everything run smarter and faster.
Programming Languages
Python is the quiet powerhouse that drives learning models and handles complex data with ease. JavaScript or TypeScript could then bring it all to life by building a smooth front end that users can actually enjoy using.
Frameworks & Libraries
- TensorFlow / PyTorch: Core engines for building and training machine learning models. Ideal for NLP tasks like denial type classification, intent detection, and sentiment analysis in appeal communications.
- LangChain / LlamaIndex: The backbone of your Retrieval-Augmented Generation pipeline, these frameworks manage document retrieval and ensure the model’s responses are factually grounded in clinical or legal evidence.
- FastAPI: A lightweight yet powerful framework for developing backend APIs. Its asynchronous design makes it perfect for handling AI inference requests and managing document processing workflows at scale.
2. The Institutional Memory: Databases
Your database architecture must handle a mix of structured, unstructured, and semantic data. A single relational database isn’t enough.
- PostgreSQL: The system of record. Stores user data, appeals, payer details, and audit logs, ensuring ACID compliance and reliability.
- Pinecone: The vector database that brings intelligence to retrieval. It stores embeddings of medical guidelines, policies, and past appeals, allowing for lightning-fast similarity search and accurate evidence grounding.
- Neo4j: A graph database built for relationships. Perfect for linking entities — like procedures, ICD-10 codes, clinical studies, and policy excerpts — to create a living “medical necessity knowledge graph.”
3. AI & NLP Tools
These tools help the system understand the language of healthcare, law, and insurance.
- OpenAI GPT-4 API / Anthropic Claude API: These are the reasoning engines. They generate coherent, compliant, and persuasive appeal letters grounded in retrieved evidence.
- Hugging Face Transformers: A hub of pre-trained models for custom NLP tasks — from Named Entity Recognition (NER) to summarizing multi-page clinical notes.
- spaCy: The industrial-strength NLP toolkit that structures the raw text extracted from PDFs, EOBs, and medical documents, converting unstructured inputs into clean, actionable data.
4. Compliance & Security
In healthcare you must build trust through real compliance and care for data. Cloud tools can help you store and track sensitive records safely while keeping audits simple. You could also use secure compute options that protect every piece of information even while it is being processed.
5. Voice AI Tools
To bring the “human touch” back to healthcare communication, voice AI bridges the gap between automation and empathy.
- Deepgram / AssemblyAI: Advanced Speech-to-Text engines optimized for noisy phone environments, perfect for transcribing payer calls and detecting denial rationales.
- ElevenLabs: State-of-the-art Text-to-Speech for generating lifelike voices that can narrate appeal summaries or interact naturally in patient-facing scenarios.
- Dialogflow CX: A conversational design platform for managing complex, multi-turn interactions, enabling an AI agent to handle phone trees, verify patient information, and converse effectively with live agents.
Conclusion
AI-driven patient advocacy platforms like Counterforce Health are changing how patients and providers experience healthcare. They help people understand their rights, give them tools to act with confidence, and make the system feel fair again. For platform owners, this isn’t just about technology. It’s a real chance to lead meaningful change while building something sustainable. At Idea Usher, we build healthcare AI solutions that are HIPAA-compliant, RAG-powered, and voice-enabled so you can innovate safely and make a lasting impact.
Looking to Build an AI App Like Counterforce Health?
At Idea Usher, we bring the technical discipline and industry insight needed to build AI health solutions that actually deliver. From secure data pipelines to evidence retrieval systems and compliance-first design, we engineer apps that are not just smart, they’re reliable, ethical, and ready for real-world impact.
Your Partner in High-Stakes AI
- 500,000+ Development Hours — Backed by a team of ex-MAANG/FAANG engineers who understand scale, speed, and precision.
- Built for Compliance — Every system we build starts HIPAA-ready, with security and governance woven into its foundation.
- From Concept to Market — We turn promising ideas into live products that attract users, partners, and investors.
Work with Ex-MAANG developers to build next-gen apps schedule your consultation now
FAQs
A1: No. Counterforce Health isn’t a medical or diagnostic app. It’s designed to help patients and providers manage appeals, understand coverage, and protect their rights. The platform focuses on advocacy and support rather than delivering clinical treatment or medical advice.
A2: On average, it takes around five to eight months to build a solid MVP. The exact timeline depends on how complex the AI system is, how deeply the voice features are integrated, and how detailed the compliance setup needs to be.
A3: Yes, it can. Many clients choose models like SaaS subscriptions for clinics, pay-per-appeal pricing, or shared revenue based on successful claim recoveries. The right approach depends on the scale and audience of the platform.
A4: The platform must meet key healthcare standards such as HIPAA, SOC 2, GDPR, and HITRUST. These ensure that patient health information stays private, secure, and fully compliant with industry regulations.